Systemic antibiotics are routinely used in equine practice to manage common diseases and infections in horses. While these medications are valuable for treating certain bacterial infections, horse owners often misuse them.
The misuse and overuse of systemic antibiotics have significant implications for the overall health of the equine population due to growing antibiotic resistance. However, these medications can also negatively impact individual equine patients, even when used correctly.
Adverse effects on the equine gastrointestinal tract are a significant concern for equine practitioners prescribing systemic antibiotics. Keep reading to learn more about how systemic antibiotics affect equine GI tract health and how proactive management can help combat these adverse side effects in your equine patients.
How Systemic Antibiotics Work
Horse owners often use local antibiotics to treat and prevent infections in minor wounds. These topical medications aren’t practical for severe cases or infectious bacterial diseases, which often require treatment with systemic antibiotics.
Systemic antibiotics are administered through oral and injectable routes and spread via the bloodstream to the target infected organ or tissues. The antibiotic must reach therapeutic levels at the site of infection to kill or inhibit the growth of the pathogen. (Haggett et al., 2010)
However, antibiotics in the bloodstream are circulated throughout the horse’s entire body, which can lead to unintended adverse effects in other systems.
Common Systemic Antibiotics in the Equine Industry
Systemic antibiotic misuse often occurs when horse owners use leftover medications to treat suspected infections without consulting their veterinarian. Practitioners use specific classes of antibiotics with different mechanisms of action to target specific pathogens and affected tissues.
Examples of systemic antibiotics commonly used in equine practice include penicillin, gentamicin, sulfamethoxazole/trimethoprim, enrofloxacin, and chloramphenicol. (Haggett et al., 2010)
Penicillin
Penicillin and other ionophores kill pathogens by damaging the cell walls of gram-positive bacteria. These antibiotics are often the treatment of choice for streptococcal infections in horses.
Gentamicin
Gentamicin is an aminoglycoside that inhibits protein synthesis in certain bacteria. It is typically given intravenously and often used to treat uterine infections in broodmares.
Sulfamethoxazole/Trimethoprim or Sulfadiazine/Trimethoprim
Known by horse owners as SMZ, sulfonamides are broad-spectrum antibiotics that interfere with DNA synthesis to stop bacteria from multiplying. These systemic antibiotics are a popular oral medication for treating infections in minor wounds.
Enrofloxacin
Fluoroquinolones such as enrofloxacin also impair bacteria replication by inhibiting DNA synthesis. These drugs are typically effective against intestinal aerobic pathogens but can damage cartilage in growing horses.
Chloramphenicol
Chloramphenicol is a broad-spectrum antibiotic used for various infections, including those caused by anaerobic bacteria. It is commonly administered orally but can be used locally as an ophthalmic ointment for ocular conditions.
Limitations of Antibiotics
Modern systemic antibiotics can effectively treat once-life-threatening conditions. However, these drugs have limitations and aren’t a good choice for all health problems and infections in horses.
Abscesses and closed infections that involve the accumulation of infected fluid within a body cavity require flushing and drainage. Antibiotics are also ineffective for chronic infections if there is foreign material or dead tissue in the body cavity or wound. These infections require debridement before medical treatment.
Antibiotics can’t treat viral infections or other diseases not caused by bacteria. However, even some bacterial infections may not respond to antibiotic treatment if the medication doesn’t reach the therapeutic levels needed to kill bacteria in infected tissue. For example, only antibiotics that can cross the blood-brain barrier can reach effective levels in the brain.
Some oral antibiotics may not absorb efficiently from the intestine into the bloodstream. If antibiotics don’t distribute from the bloodstream to the infected tissue, they can’t treat the infection. Some bacterial types are also resistant to particular antibiotics. (Maddox et al., 2015)
How Antibiotics Affect The GI Tract
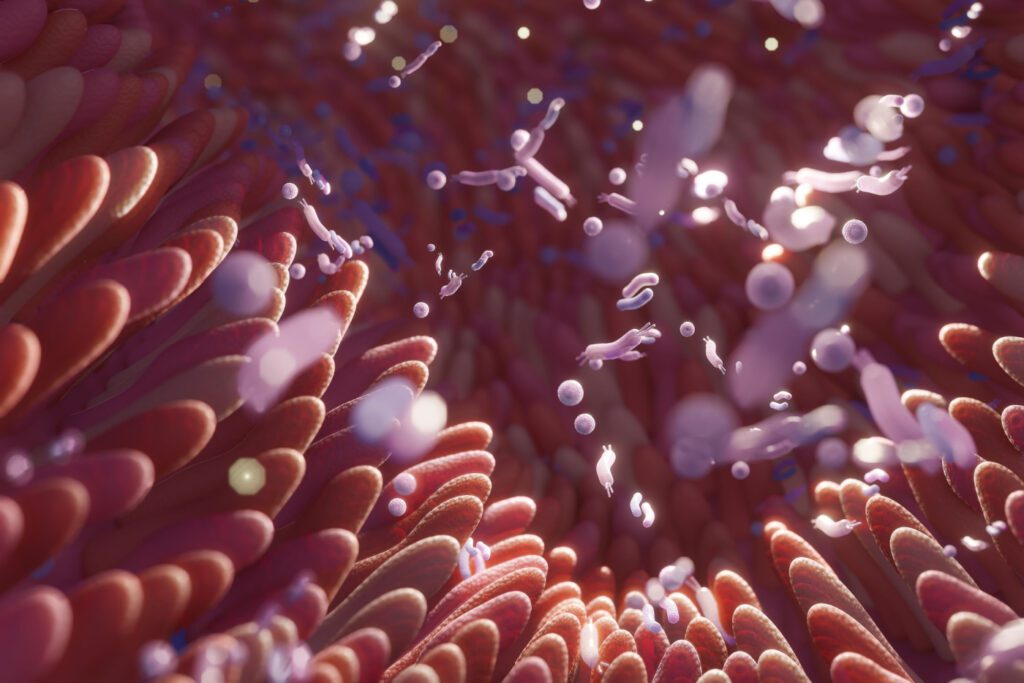
Systemic antibiotics must be used cautiously in horses due to the risk of complications to the equine gastrointestinal tract. These medications can have unintended consequences on good bacteria species that horses rely on for health, immunity, and digestion.
The equine hindgut houses large populations of microbes that are critical for forage fermentation and digestion. This microbiota is vulnerable to disruption by antibiotic use. Imbalances in the microbiota associated with antibiotics can contribute to antibiotic-induced colitis. (Costa et al., 2015)
Mild diarrhea due to a disturbance of the gut microbiota is a common side effect of antibiotics. However, severe disruptions can be life-threatening. While some antibiotics have a higher risk of colitis, gastrointestinal disturbances can occur with any systemic antibiotic. (Costa et al., 2015)
How to Combat Negative Side Effects
Practitioners and horse owners should prioritize maintaining microbiota balance during antibiotic treatment to limit the risk of adverse GI tract health side effects. Healthy digestive function and good nutrition are essential for supporting immunity to fight infection.
As a result, digestive problems associated with antibiotic use can also affect treatment outcomes in equine patients. But even if treatment of the infection is successful, GI tract disruptions can lead to ongoing digestive health problems in horses after the course of antibiotics ends.
Consider recommending a nutritional program that provides additional digestive support during and beyond antibiotic treatment to help maintain digestive health in equine patients.
Using SUCCEED Alongside Antibiotics
The high-quality ingredients in SUCCEED help maintain gastrointestinal health in horses undergoing treatment with systemic antibiotics. Unlike some medications or supplements, SUCCEED is safe to use as a complement to medicine and doesn’t have harmful interactions with antibiotic drugs used in horses.
Prebiotics in SUCCEED Veterinary Formula encourage the growth of good bacteria that might be affected by antibiotic treatment to restore a balanced gut microbiota.
But digestive support shouldn’t stop after patients finish treatment. Ongoing nutritional support for the entire equine gastrointestinal tract supports overall health and immunity, which helps maintain the horse’s natural defenses against pathogens.
References
- Haggett, E. et al. Overview of the use of antimicrobials for the treatment of bacterial infections in horses. Equine Vet Ed. 2010
- Maddox, T. et al. Antimicrobial resistance in bacteria from horses: Epidemiology of antimicrobial resistance. Equine Vet J. 2015.
- Costa, M. et al. Changes in the equine fecal microbiota associated with the use of systemic antimicrobial drugs. BMC Vet Res. 2015.