A range of disorders can occur in the equine gastrointestinal tract, often varying widely in causes, symptoms and treatments necessary for recovery. Post-mortem research has shown the incidence of colonic ulcers to be on the rise over recent years, from 63% in a 2004 study to as high as 84% in studies carried out from 2007 to 2011. In addition, a high degree of overlap between foregut and hindgut issues has also emerged.
Given these trends, comprehensive evaluation of gastrointestinal tract health is vital for the veterinarian to formulate an accurate diagnosis and effective treatment plan when ulcers or other pathological conditions of the GI tract are suspected.
Developing Our Understanding of Colonic Ulceration
Significant advances in equine colonic ulcer research over recent years has led to a better understanding of this condition and a growing appreciation for its significance. While more research is certainly needed to build a greater understanding of the etiology of colonic ulcers, it has become clear that the existence of ulcers in the colon reflects a wide range of possible pathologies.
An awareness of the symptoms of colonic ulceration can be extremely useful when considering clinical presentation, and several signs are now becoming more accepted:
- A loss of performance, weight, condition or appetite
- Training issues such as a reluctance to flex laterally through the body, extend, collect
- Girthing issues and/or sensitivity of the flanks, behavioral problems
- Ventral edema, laminitis, diarrhea, endotoxemia, colitis, bouts of colic, hindlimb lameness, hypoalbuminea, anemia
The use of a diagnostic test in helping to identify colonic ulcers becomes even more advantageous when outward signs could be mistaken for a range of other problems such as EGUS, behavioural problems, and even lameness. Clearly, a misdiagnosis can be costly economically and hinder appropriate treatment necessary for an effective recovery. In fact, given that the primary treatment protocol for EGUS is the use of some form of proton pump inhibitor, it is possible that treating ulcers in the stomach when, in fact, they are in the colon, may actually be doing harm.
Hindgut, Foregut or Both?
While awareness of colonic ulceration is growing alongside the widely recognized incidence of gastric ulceration, there exists the real possibility that a horse may be suffering from both.
In a 2003 study of 180 performance horses at a Texas abattoir, we found that 87% of the horses had gastric ulceration and 63% had colonic ulceration; an overlap of 54% indicating that over half of these horses had both.
Hindgut and gastric ulcers differ in their pathophysiology and so require differing treatments. Information on the origin of blood loss from ulceration therefore becomes paramount when implementing an appropriate and effective plan for recovery.
Equine Fecal Blood Test for Differentiating Gastric and Colonic Ulcers
In conjunction with other diagnostic methods, such as clinical history and presentation, CBC, blood chemistry and fecal egg counts, the SUCCEED Equine Fecal Blood Test proves to be a highly valuable tool in the differential diagnosis of GI tract disorders.
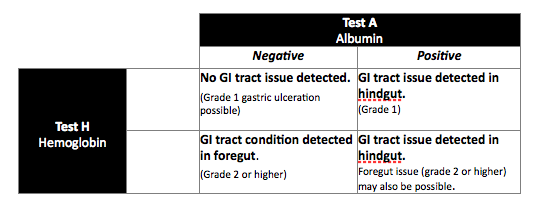
The FBT works by detecting equine hemoglobin and albumin within a fecal sample. These two blood markers provide two important pieces of information to support a differential diagnosis.
First, albumin and hemoglobin reflect two different levels of severity of injury. Hemoglobin is associated with injury where whole blood loss occurs, while albumin can leak from a compromised basement membrane without whole blood loss (i.e., a “weeping” lesion). Thus, the presence of hemoglobin reflects a more severe injury than the presence of albumin alone.
Second, albumin and hemoglobin in feces reflect different injury locations in the GI tract. Because albumin is broken down by digestive enzymes in the duodenum, albumin present in fecal matter must have originated in the hindgut. Hemoglobin, on the other hand, is a durable molecule, resistant to the enzymes and acids in the gut. Hemoglobin in feces may have originated anywhere in the GI tract. Thus, these two markers can help the veterinarian differentiate between foregut and hindgut problems.
The SUCCEED FBT can aid diagnosis of hindgut vs. foregut issues to enable a more targeted treatment strategy and, subsequently, a quicker recovery.
A positive FBT result is not a confirmation of ulcers. It is a confirmation of where in the GI tract an issue is present that may include ulcers. As such, it should be used in conjunction with other diagnostics when ulcers are suspected.
The FBT is invaluable in helping to diagnose and monitor treatment/recovery of many GI tract issues, which may commonly include:
- Lawsonia Intracellularis, Salmonellosis, Clostridium and Streptococcus
- Hypoalbuminea, Hypoproteinemia, Parasitism, IBS/IBD, Colitis, Starch-induced Laminitis, Colic and Protein Losing Enteropathy
To purchase the FBT contact your veterinary supply distributor. For more information on using the FBT for the diagnosis of hindgut and gastric conditions contact Freedom Health LLC.